By mapping millions of cells, VCU researchers are gaining new insights into pediatric respiratory conditions
Originally published to VCU News.
Researchers at Virginia Commonwealth University’s School of Dentistry are part of a multinational effort to map the millions of cells that make up respiratory systems in children. Creating an atlas of these systems in unprecedented detail will allow health experts to better understand and treat diseases and respiratory conditions that commonly impact pediatric populations, such as viral and bacterial infections, asthma and allergies.
This effort is one of 14 projects selected for Scale Biosciences’ 100 Million Cell Challenge, a program dedicated to advancing single-cell genomics research by supporting large-scale initiatives that address critical challenges in global health. As one of the winning projects, this initiative will be fully funded and supported by Scale Biosciences, the Chan Zuckerberg Initiative, Ultima, Nvidia and BioTuring.
“The lungs, oral cavity and nasal space are essentially one interconnected cul de sac of breathing. This includes all the tissues and fluids that interact with the air you breathe. These areas are often the first place of contact for viruses, bacteria, pollutants and allergens,” said Kevin Matthew Byrd, D.D.S., Ph.D., assistant professor at the VCU School of Dentistry’s Philips Institute for Oral Health Research and one of the project leaders.
While the research community has made great strides in mapping the cells that make up respiratory systems in adult bodies, less is understood about these systems in younger populations.
“Children are often more vulnerable to airborne pathogens and other substances than adults since their immune and respiratory systems are still developing,” Byrd said. “Mapping these systems at a cellular level will give us new insights into how we can better treat diseases and respiratory conditions in pediatric patients.”
Byrd has now assumed leadership of this effort after it was directed for more than three years by James S. Hagood, M.D., professor at the University of North Carolina’s School of Medicine and director of the Program for Rare and Interstitial Lung Disease at the UNC Children’s Research Institute and Marsico Lung Institute. Other partners on this project include researchers from Duke University, the Institute for Stem Cell Science and Regenerative Medicine in India, Pontifical University of Rio Grande do Sul and the University of Sao Paulo in Brazil, and Helmholtz Zentrum München in Germany.
This project began in 2021 when the research team received a $3.5 million grant from the Chan Zuckerberg Initiative to collect samples of tissue in the nose, mouth and airways of pediatric patients across all ages. This effort has since compiled more than 500 samples from six countries – Brazil, Germany, India, Malawi, Australia and the United States.
The researchers also collected samples of cells and tissues impacted by at least 10 diseases, including cystic fibrosis, bronchiolitis obliterans syndrome and chronic obstructive pulmonary disease, from children and adults.
With support from the Scale Biosciences’ 100 Million Cell Challenge, the research team has been sequencing the cells within these samples at a significantly accelerated rate.
“The field of single-cell genomic sequencing has changed so much just in the last 10 years. We’ve reached a point where we can analyze millions of cells instead of thousands, which provides new possibilities for understanding and treating diseases.” Byrd said. “By partnering with these companies, we’ve been able to efficiently sequence an incredibly large amount of cells and create a vast library of information on pediatric health.”
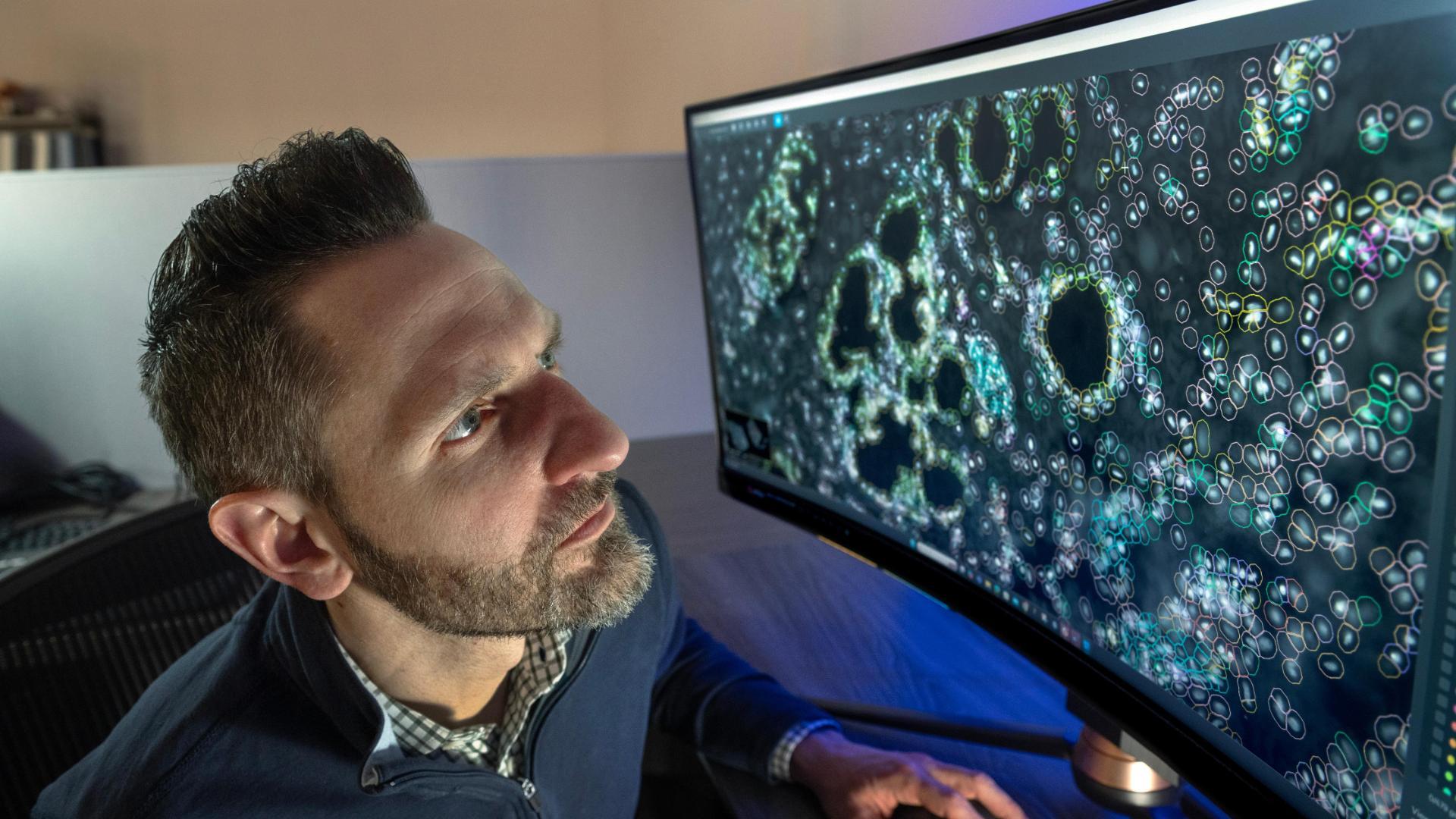
Using artificial intelligence, the researchers will develop a virtual map of the cells that make up the mucosal surfaces of the nasal and oral cavities, throat and lower airways in pediatric subjects. They will also include information on how these cells behave, how they interact with each other and how they are impacted by different disease states. The researchers envision that this data could also be used to identify existing drugs that could be effective for treating other diseases.
“Using AI, we can scan through disease mechanisms and identify drugs that have already been approved to treat one type of disease but could potentially be effective in treating additional conditions,” Byrd said.
This resource will serve as a foundational model to share new insights into how respiratory systems develop through early childhood and adolescence, as well as help health experts better understand the cellular mechanisms that drive disease and other conditions. Such knowledge could ultimately inform new developments in diagnostics, prevention strategies and therapies for pediatric respiratory health.